Automating building systems reduces management burdens and saves energy. However, in healthcare, maintaining specific parameters for certain spaces is essential to providing optimized care. Automated control systems maintain the environmental requirements for critical rooms effortlessly, making the spaces safer and healthier for patients and clinicians.
Critical Environments in Healthcare
Healthcare facilities have multiple spaces that require tight control over environmental factors, including maintaining air quality, temperature, pressure, humidity, and more. Meeting these requirements can become challenging, but facilities must keep these critical environments consistent for the health and safety of patients and staff.
For example, operating rooms need to maintain the cleanliness of the space and airflow that reduces pathogen transmission. Having an automated control system to create airflows that prevent germs from moving outside the room is critical to keeping the rest of the hospital sanitary.
Another instance of critical environment requirements is patient rooms that must maintain specific humidity and temperatures for patient comfort and high indoor air quality. In isolation rooms, air distribution needs to ensure patients have fresh air and keep the air from flowing out to the rest of the hospital.
Laboratories, pharmacies, and testing areas need proper pressures and airflow to isolate the air in the room and prevent contamination of areas outside the space. Additionally, lab technicians need access to adequate lighting to work, which may require lighting the spaces 24 hours of the day to accommodate overnight shifts. Lighting control systems reduce energy use for times when a lab is unoccupied.
Factors for Critical Room Control Consistency
Critical environments need consistency in their environmental controls, and each space has specific needs. Some factors that critical environments may need to control include indoor air quality, temperature, air exchanges, humidity, and pressures:

1. Indoor Air Quality
Indoor air quality for a healthcare facility can directly impact the health and wellness of everyone in the building. For example, failing to control for pathogens spreading through the HVAC system could contribute to staff needing more sick days or patients experiencing secondary infection. Critical environments must consider preventing the spread of infectious materials. With Engineered Infection Protection (EIP) from SitelogIQ in your HVAC system, you can reduce contaminant spread from inside or outside the facility.
2. Temperature
Temperature control inside hospitals and other healthcare facilities ensures the comfort of staff and patients. In locations that experience extreme heat in summer, such as Texas, or extreme cold in winter, such as the Midwest, HVAC bills can shift dramatically with the change in seasons. Regulating indoor temperatures through automating the HVAC system ensures continued indoor comfort with less of an impact on energy use.
The standards for healthcare facility temperatures in specific areas fall under the ANSI/ASHRAE/ASHE 170-2017 standard. This guideline outlines specific ranges of temperatures that areas of healthcare facilities should maintain when occupied. The guideline also allows for some spaces to have temperature adjustments to save energy when the spaces are empty. For example, the design parameters for temperature are uniquely defined for dozens of specific patient care areas, diagnostic and treatment areas, and patient support areas.
3. Air Exchanges
Maintaining proper air exchanges gives constant fresh air supplies into a healthcare facility’s critical environments. In places such as labs and operating rooms that require air to be contained in the rooms, air exchanges have to account for a way to safely ventilate the room without exposing the rest of the facility to contamination. Options may include creating air curtains and pressure differentials, or using airflow and filtration to keep the entire facility protected from internal air contamination.
Regulations from ANSI/ASHRAE/ASHE 170-2017 outline the specific number of minimum air exchanges per hour and whether a critical environment has permission to vent its air to the outside. There are two air changes per hour (ACH) metrics that are noted but compared as equal — minimum outdoor ACH and minimum ACH. For example, depending on the laboratory type, the air changes per hour may range from six to 10 and exhaust the air to the outside. Other critical environments, such as operating rooms, require 20 air changes per hour with four or more of them being a complete change with outside air to establish a minimum flow of fresh air into the room.
4. Humidity
Humidity levels matter more than many people realize. For example, when humidity is too low, individuals may have dry skin or feel thirsty. If the humidity rises too high, mold can breed, causing allergen problems and making the space feel uncomfortable. Keeping the humidity controlled promotes a healthier space for everyone and greater comfort.
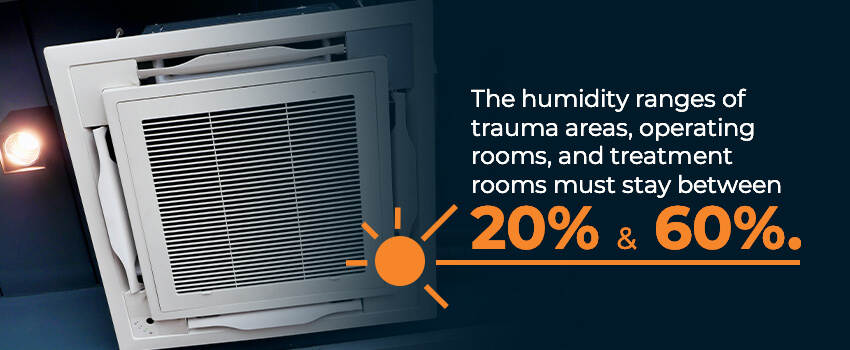
One example of the consequences of failing to control for humidity levels and proper air handling occurred at Seattle Children’s Hospital in a series of mold outbreaks starting in 2001. The outbreaks killed six individuals and sickened another 14. The facility failed to fix their operating room air handling system that allowed the spread of Aspergillus mold that originated with a nitrogen tank. Since the incidents, the hospital has faced several legal battles.
Just as ANSI/ASHRAE/ASHE 170-2017 regulates temperatures, the standard also outlines humidity levels for healthcare facilities. Most places around a hospital have a maximum of 60% relative humidity allowed, except for the emergency room waiting area and physical therapy sites, which have 65% as their maximum humidity levels. Trauma areas, operating rooms, and treatment rooms have ranges of humidity that must stay between 20% and 60%. Automating humidity controls can ensure these spaces stay safe, comfortable, and compliant with industry standards.
5. Pressures
Pressure control of rooms can help prevent cross-contamination of spaces in a healthcare facility. The World Health Organization (WHO) recommends a pressure differential of 15 pascals between a cleanroom space for pharmaceutical manufacturing and a non-clean space.
Another instance of pressure making a difference in healthcare is the application of negative pressure by healthcare facilities handling COVID-19 patients. The negative pressure allows for more incoming fresh air from outside and more air exchanges. Some facilities chose to install pressure that would convert areas of the hospital into negative pressure zones from a centralized control computer. Existing facilities can choose to upgrade to such a system or retrofit their existing spaces to meet possible future infection control needs.
Though not a requirement, the most recent industry standards governing healthcare facility HVAC systems permit facilities to plan for the future by retrofitting standard patient care rooms into airborne infection isolation rooms through pressure and airflow changes in the room.
Benefits of Automation in Healthcare
As seen with the COVID-19 pandemic, having an automated building control system can permit quick adaptations to sudden changes in needs for controlling infection spread. Automation serves as the first step in integrating the Internet of Things (IoT) in hospital management and offers some of the following advantages:
1. Improved Patient Care Conditions
Patients benefit from healthcare facilities that use automated building systems in several ways. First, care conditions improve because operating and isolation rooms prevent disease spread through applications of pressure and air exchanges. Other patients in the facility who have weakened immune systems due to diseases or operation recovery also have lower chances of contracting an airborne infection from a patient in another room when the facility uses HVAC-based isolation methods properly.
Those in patient rooms can stay more comfortable in climate-controlled rooms. Better temperature control in patient rooms ensures patients don’t feel too hot or cold during their stays. Proper humidity levels and air quality control prevent allergens and other airborne agents, including infectious diseases, that could sicken patients.
2. Safer Laboratories
Laboratories and testing areas heavily rely on proper airflow to keep chemicals, airborne pathogens, and gases isolated to the room. Most laboratory spaces need negative pressure, with the exceptions of pharmacy and media transfer labs that need positive pressure. These negative pressure spaces need air exhausted to the outside during air changes to maintain pressure and protect the rest of the hospital.
Air pressure and airflow automation to meet the ANSI/ASHRAE/ASHE 170-2017 air exchange and ventilation requirements keeps a lab working space safer by isolating the air and anything in it to the laboratory and keeping it out of the rest of the hospital.
3. Lower Energy Costs
In healthcare facilities, energy costs can account for 50% of the building management budget. Controlling those costs by regulating lighting, heating, and cooling can make significant dents in the overall operating budget. Automating controls allows for temperature, humidity, and lighting of occupied critical environments at required levels while reducing energy use when those spaces are empty. Automatic controls can detect room occupation, shutting off lights or changing room temperatures when the space is empty, thus saving energy and lowering building operating costs.
4. More Environmentally Conscious
Reducing energy use also has a more environmentally conscious side. It can reduce the overall need for fuel, which lowers the facility’s impact on the environment. One step toward a greener healthcare facility starts with automatic building controls. Other means include incorporating solar panels or other energy-savings methods. The United Health Centers in the Central California Valley worked with SitelogIQ to incorporate solar panels into three of its sites with four planned to reduce its environmental impact.
Other aspects of greener building and greater energy efficiency could lead to LEED certification for a facility. Healthcare sites could also participate in working toward the 2050 goal from the World Green Building Council to have 100% Net Zero Energy Buildings.
Long-Term Impacts of Healthcare Control Systems
Long-term impacts of healthcare control systems provide continued advantages for the facility long after installation. The benefits include:
- Better capacity for a greater variety of care: Improving care for patients may require a healthcare facility to make sudden changes to its environmental controls. For example, the building management system in the Children’s Hospital of Philadelphia allows for 150 rooms, two floors, and three wards to instantly switch to airborne infection isolation areas without making major changes other than changing control settings. This ability ensures the flexibility of the facility to provide high-quality care in emergencies without wasting energy maintaining such negative pressure zones when not needed.
- Maintaining regulatory standards for healthcare critical environments: Regulations can change quickly. For example, the ANSI/ASHRAE/ASHE 170 standard undergoes perpetual evaluation and change. Because the committee constantly evaluates changes in technology and updates to care needs, they can make changes to the environmental requirements for healthcare facilities at any time. Manual controls do not allow quick changes as the standards update. Automated controls permit rapid updates to all critical environments in the healthcare facility and non-critical spaces.
Expert Maintenance of Critical Environment Automation
During evaluation, installation, and maintenance, automated controls need experts to ensure they meet regulation needs and the challenges of critical environments in a hospital. The SitelogIQ energy consultants provide turnkey solutions by designing solutions, providing materials, installing the project, and monitoring use.
Through regular monitoring and evaluation of the critical environment automated system, we provide healthcare facilities with the information needed to make adjustments required to update their facility to any regulatory changes or to reduce energy. We also examine the facility and its energy use to identify areas that could improve with better controls or automation.
With the help of energy experts who know the needs of healthcare facilities, especially the specifics needed for critical environments, a healthcare facility can save money, offer better patient care, reduce energy use, and have a safer workplace for its staff.
Contact SitelogIQ for More Information on Automated Healthcare Solutions

Find out more information about how to have a medical automation system set up and installed in your healthcare facility. We help your critical environments stay safe and meet regulatory requirements through automated building controls tailored to specific rooms. Contact us at SitelogIQ for more information on our building automation services and how to get started today.